Context:
Tracheostomy care across the UK is associated with significant standard variation, leading to avoidable harms, delays in weaning, and unnecessary use of NHS resources. Poor infrastructure, lack of formal tracheostomy teams, and inconsistent staff training contribute to long lengths of stay in critical care and increased demand on frontline services. These challenges place a considerable financial and operational burden on the NHS.
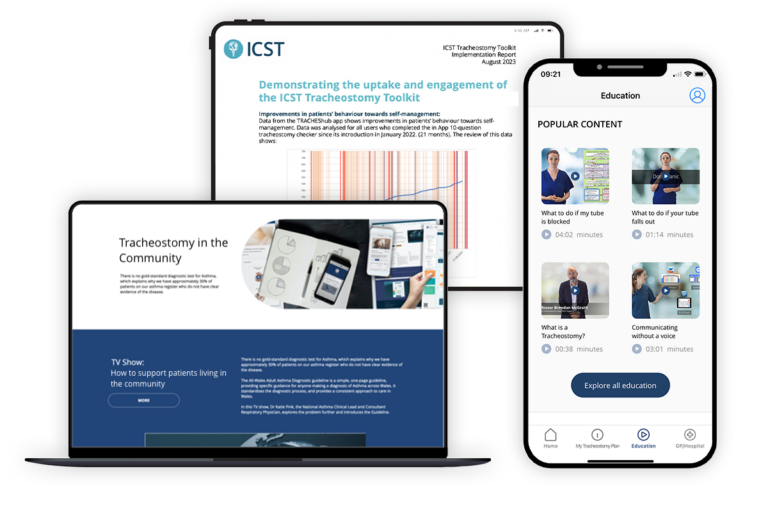
To tackle this, ICST partnered with NHS Wales, NHS England, the National Tracheostomy Safety Project (NTSP), Great Ormond Street Hospital, Royal Brompton Hospital, and the College of Paramedics to standardise tracheostomy care across the entire system. The ICST Tracheostomy Toolkit empowers patients, upskills healthcare professionals, and provides national-level data insights, helping to deliver safer, more efficient care while reducing demand on services.
Solution:
TRACHES Toolkit
The toolkit offers digital and practical support for patients, professionals, and organisations, using implementation science and behaviour change methodologies to achieve adoption, consistency, and improved outcomes without adding strain to services.
The TRACHES toolkit is structured into four layers:
1
Patient Self-Management Apps
2
Healthcare Professional Platform
3
Organisational Platform
4
Commissioner Data Reporting
By using implementation science and individual behavioural science methodologies, the toolkit achieves reach and adoption whilst achieving outcomes. This approach ensures seamless system installation without the need for additional resources or staffing. By practically supporting existing services, rather than imposing fundamental change, the toolkit minimises resistance, ensures sustainability, and achieves population-level reach and scalability.
Outcomes:
Tracheostomy Toolkit
The digital approach to standardising tracheostomy care has led to measurable improvements in patient outcomes, system efficiencies, and cost savings
Improved patient outcomes and reduced healthcare utilisation
Median time to cuff deflation reduced from 10 to 6 days
Median time to decannulation reduced from 19 to 17 days
Median length of stay reduced from 54.5 days to 46 days, resulting in 4,573 fewer bed days
Significant reduction in adverse events
Patients experiencing at least one adverse event reduced from 21.1% to 13.4%
Moderate adverse events reduced from 35% to 2%
No severe incidents or tracheostomy-related deaths for two years
Near-universal reach and measurable cost savings
Toolkit implemented at scale, supporting national improvement programmes
Potential savings of over £1.9 million per hospital trust annually through improved outcomes
No variation in uptake by geography or deprivation index, ensuring equitable access
The toolkit is now being implemented across the UK.
"The TRACHES toolkit has been central to our work in NHS Wales, and I believe its effectiveness has been well demonstrated in the improvements in patient care observed, far exceeding the accomplishments that we could have achieved through other methods. We are confident that through this partnership we can continue to drive improvement at scale"
Paul Twose
Clinical Lead for Tracheostomy, Cardiff and Vale UHB